Cataract Surgery
Mr Venki Sundaram has established himself as a leading provider of cataract surgeries having trained & gained experience at world-class institutions including Oxford University and Moorfields Eye Hospital and has treated & restored vision to thousands of patients over his career. At Herts Eye Surgeon, we ensure Excellence in Eye Care at every step of your journey.
To book your initial consultation speak to a member of our team today.
What is a cataract?
A cataract is a clouding of the lens in the eye, a natural ageing process that occurs in all eyes over a certain age. If a cataract forms at a younger age, this could be down to other conditions such as diabetes, inflammation of the eye, steroid use or trauma.

How do I know if I have a cataract? What are the symptoms?
Symptoms tend to occur over several months or years and some may be less severe or noticeable than others. These include:
- Gradual reduction/clouding of vision
- Less clarity of colours and objects
- Glare, especially when driving at night or in exposure to bright lights
At what point is cataract surgery advised?
Cataract eye surgery is recommended when the level of vision due to the cataract is interfering with everyday life. For example, if vision has dropped below the legal driving limit, reading or watching TV is becoming increasingly difficult or you are unable to enjoy your typical hobbies and activities, surgery would be advised to improve quality of life.

What does cataract surgery involve?
Cataract surgery is one of the most commonly performed operations in the world, and has an excellent success rate and safety record. Treatment can be broken down into three stages: before, during and after.

What are the risks of cataract surgery?
Cataract surgery is an extremely successful and safe procedure. However, as with any operation inside the eye, it will always carry a certain risk.
The risks include:
- 1:1000 – severe or permanent loss of vision due to acute infection or bleeding within the eye.
- 1:100 – additional surgery required to rectify a problem that occurs during the cataract operation.
- 1:10 – laser treatment at a later stage due to clouding of the lens capsule behind the implant.

A lens implant that is inserted into the eye, replacing the natural lens (Image courtesy of Rayner)
Are there different types of lens implants?
A lens implant is placed in the eye during surgery, the power of this implant is calculated from measurements made prior.
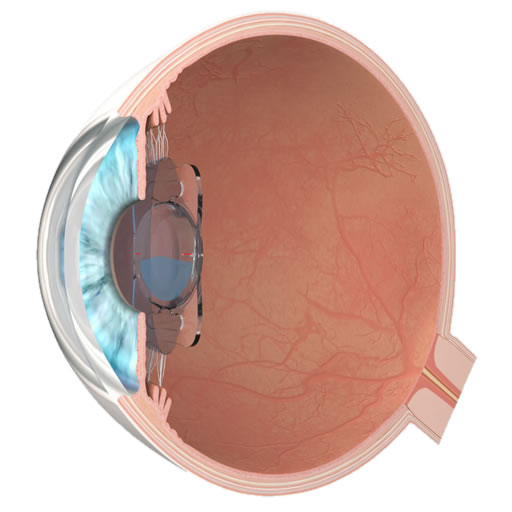
An illustration of multifocal lens implant in the eye (Image courtesy of Oculentis)
The main types of lens implants used are:
Monofocal lenses – a fixed focusing power enabling people to see most objects in the distance without glasses.
For fine tuning of distance vision, a weak spectacle prescription may be required, and patients will need to wear reading glasses afterwards.
Enhanced monofocal lenses – gives excellent distance and also some intermediate range vision, which is useful for looking at a computer screen and some larger near vision text.
Multifocal lenses – different focusing powers built within them allowing people to have good distance, intermediate and near vision without glasses.
These do not suit everyone and may cause some quality problems, therefore, their use needs to be fully discussed prior to implantation.
Toric lenses – used if a patient has a moderate to high amount of astigmatism (which is an additional curvature of the cornea).
They are able to correct astigmatism and reduce the need for wearing distance glasses after surgery, however, reading glasses may still be required.
Various lens implants are available depending on your personal requirements and visual needs. Mr Sundaram can explain the options available so that you are able to choose which one suits your particular wishes.
Why Venki Sundaram is a trusted surgeon…
Highly trained in private cataract eye surgery in Hertfordshire, Venki Sundaram has extensive experience (as well as interest) in performing this surgery on patients with additional retinal conditions alongside cataracts; acquired at Moorfields Eye Hospital. His impressive results are well within the standards set by the Royal College of Ophthalmologists and he performs every surgery with the highest professional manner, passion and care.

“I was fortunate in becoming a patient of Mr Sundaram, charming, caring, a man who listens and is easy to talk to. After two cataract operations, I am delighted.”
PB, Nov 2017
